Every 2 minutes a woman is diagnosed with breast cancer in the United States. Women with very “dense breast tissue” are four times more likely to get breast cancer than women with fatty breasts.
While breast density is not related to breast cancer survival, having dense breasts can make detecting cancer, especially in the early stages when it’s easiest to treat, challenging.
What is breast density?
Dr. Julie DiSano, a surgeon at Southwestern Vermont Medical Center (SVMC) and program lead of SVMC’s High Risk Breast Cancer Program said, “Breasts are made up of breast tissue, which includes the milk ducts, fat, and lobules, or glandular tissue. In addition, there’s quite a bit of connective tissue that holds the breast together and in place.
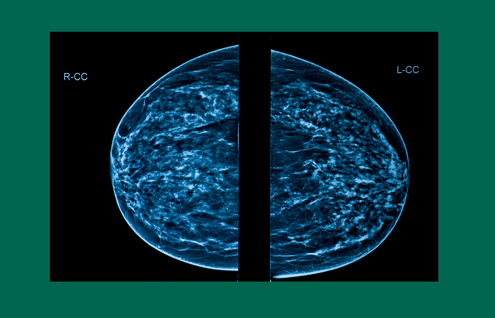
“When a breast has more breast and connective tissue than it does fat, it’s considered a dense breast. While they don’t feel different or look different to the naked eye than a non-dense breast, dense breasts do look different on mammogram imaging.”
Why it matters
While dense breasts are not considered abnormal—40% to 50% of women ages 40 to 74 have them—they are associated with an elevated risk of developing breast cancer. A primary reason for that is that dense breast tissue can make it difficult to see abnormal growths in mammograms that may be cancer.
“Both cancer and fibrous tissues appear lighter gray on a mammogram,” says DiSano, “which can make it very hard to read the imaging. But fortunately, there are alternative imaging options available.”
What to do if you have dense breasts
For women with dense breasts and a higher risk of breast cancer based on their personal and family history, regular breast cancer screenings include annual mammogram and consideration for additional imaging in the form of an MRI (magnetic resonance imaging). At SVMC, we have been doing digital mammography with 3D tomosynthesis since 2021. The addition of tomosynthesis has been shown to increase mammography cancer detection rates in early studies.
“Like mammograms, MRIs are non-invasive screenings, but,” says DiSano, “cancers enhance differently on MRI, making MRI a more sensitive test for identifying breast cancers. This means that a breast cancer can be identified earlier with the addition of MRI.”
“Dense breasts are one of the reasons for a screening callback,” says DiSano. “As alarming as getting a callback for more imaging may be, more often than not, it’s just a precautionary measure. In addition to dense breast tissue, a mammogram may also reveal cysts or calcifications within the breasts. In fact, fewer than 1 in 10 women called back for more tests are found to have cancer.”
Dr. DiSano also notes that callbacks are especially common after a first mammogram as there’s no previous mammogram with which to compare to the new imaging. Callbacks are also more common in women who have not gone through menopause.
“The most important thing for all women, regardless of their breast density, is to get yearly mammograms,” says DiSano. “Early detection is the strongest predictor of a good outcome if breast cancer is detected.
Dr. Disano is a general surgeon and the program lead of the High Risk Breast Cancer Program, offered by SVMC General Surgery. To learn more about your risk, ask your primary provider for a referral to SVMC’s High Risk program. Patients who qualify will meet with a surgeon to review their risk status and make a plan.